Vascular Access and Haemodialysis Study Day
27th September 2024
 |
By Rachel Norris BSc DMU AVS and Rachel Deadman BSc AVS
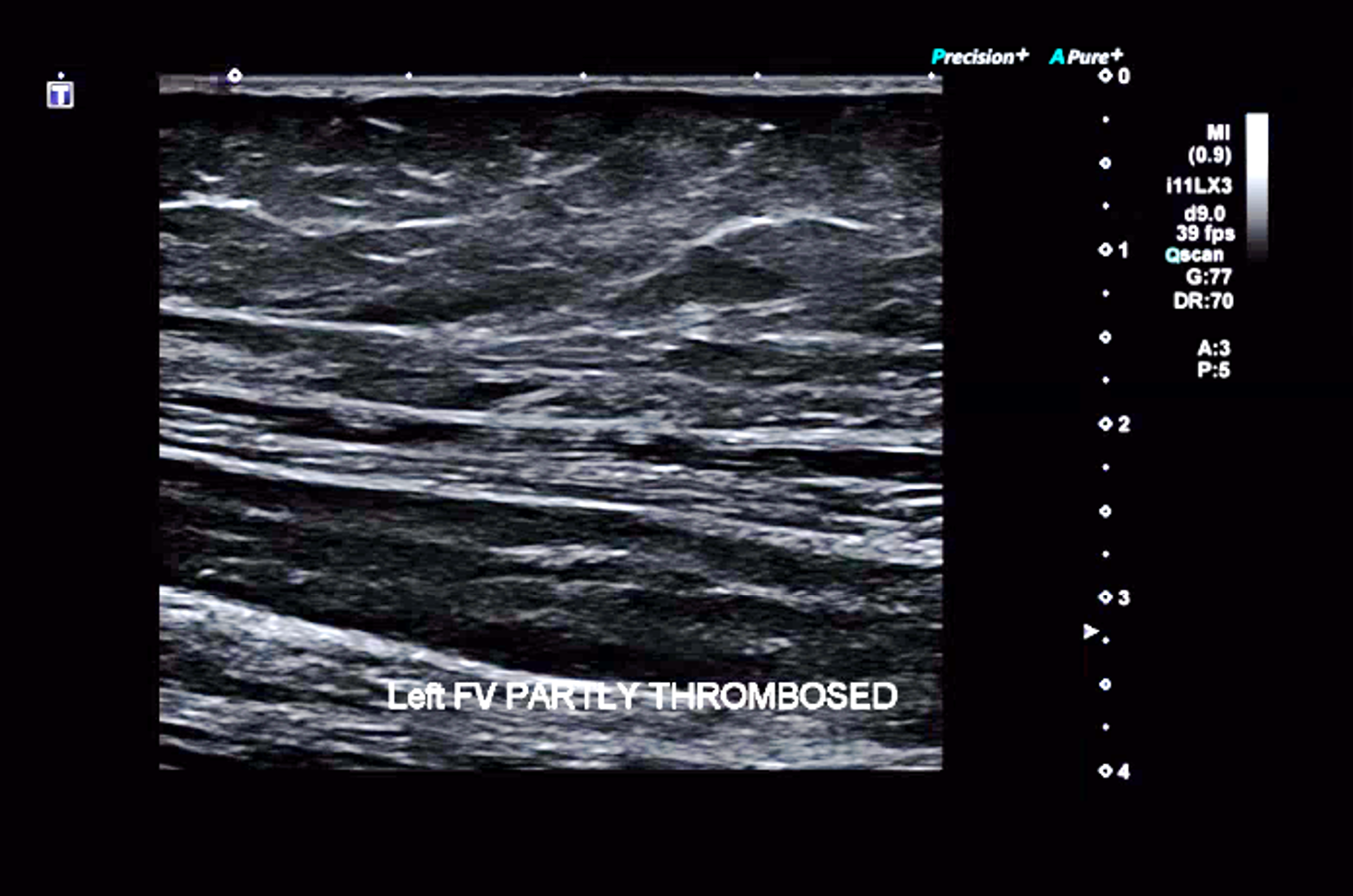
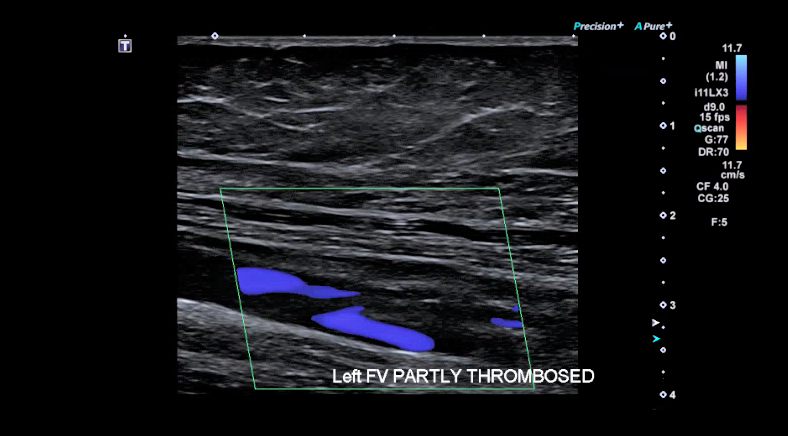
I think everyone in a Vascular Studies Unit running a DVT service in the UK and Ireland has probably noticed that their positive diagnostic rate for DVT during the covid epidemic and in the first quarter of 2022 has been at seemingly much higher levels compared to the pre-covid era.
Covid-19 has already been identified as a risk factor for myocardial infarction and stroke (1) The increased risk of DVT due to Covid-19 infection had also been linked to those patients with very severe Covid-19 infection. (2) It was then important to find out whether milder Covid-19 infections could also cause increase in DVT incidence, but this required very large-scale population research in order to generate any meaningful significant differences between groups of subjects. Fortunately, recent research articles have been published that have helped to support the clinical suspicion of DVT risk associated with Covid-19 infection.
In an article published in the BMJ (3) in April 2022, a research team in from Umea University in Sweden, examined data for over a million people in the country who tested positive for Covid-19 between February 2020 and May 2021.They were also compared to a cohort of more than four million people who had not contracted the virus, and then matched for age, sex and county of residence. This gave a 1:4 ratio of Covid-19 patients to matched controls.
Increased risk of first time DVT with Covid-19
During the study period 1761 participants with Covid-19 had a primary event DVT. No increased risk was detected in females relative to males.
In the matched cohort study a primary event DVT occurred in 401 Covid-19 patients giving an absolute risk of 0.039% and 267 control patients had a DVT giving a risk of 0.007%.
However, looking at the figures in more detail, the relative risks of DVT occurrence is 5 times higher in the group with Covid-19 compared to controls. This risk was maintained over the 30 days post Covid. Even up to 70 days post infection, the risk was much higher in Covid-19 infected patients.
The risk was higher in the first pandemic wave compared to 2nd and 3rd waves and also risk was higher with more severe Covid symptoms. Long term anti coagulation prior to Covid did NOT appear to be protective.
Increased risk of PE with Covid-19
3267 patients had a first-time pulmonary embolism (PE, blocked vessel in the lung). A first PE occurred in 1,761 patients with Covid-19 (absolute risk 0.17%) and 171 without (absolute risk 0.004%).
The risk of having a PE was 36 times higher in the Covid-19 group in the first week and 50 (range 46-53) times higher in the second week compared to the control cohort. This risk was maintained up to 110 days (3-4months) after infection.
Some increased risk was noted in the incubation period and 30day pre-positive period as well which may require more investigation as to the reasons why this was occurring. The authors thought it likely that the subjects had been infected before day 0 (of a first positive test) and also that day 0 was not included in the post infection figures and had been included in analysis for the pre-infection period.
More risk was noted with being male, in patients 50-70, with more severe Covid disease and ICU admission. Again, as with DVT, risk of having a PE was higher in the first wave compared to the 2nd and 3rd waves. But it seemed less evident in these findings that the Covid infection wave type was a risk factor as in later phases of the disease in wave 3, the risk of PE was higher than in wave 1.
They did find that long term anticoagulation WAS protective against PE.
 |
 |
Increased risk of bleeding events with Covid-19
7927 patients had a bleeding event. A first bleed occurred in 1,002 patients with Covid-19 (absolute risk 0.10%) and 1,292 without (absolute risk 0.04%).
So, patients with Covid-19 had just over a three-fold increased risk of bleeding in the first week after covid-19 and were 2.75 times more likely to have a bleeding event in the 2nd week. This risk was maintained at a doubling of risk 2 months after infections and also in the peri-infection period.
In summary
The study authors commented that, compared with the control period, risks were significantly increased in the 3 months after Covid-19 infection for DVT, 6months for PE and 2 months for bleeding. After controlling for a range of factors, they found a five-fold rise in DVT risk, a 33-fold rise in risk of PE, and an almost two-fold increase in bleeding risk in the 30 days after infection.
Even mild, non-hospitalising Covid-19 disease increases risk of these events.
How does this study change future management and is more study needed?
Apart from the obvious awareness of the higher risk of DVT, PE and bleeding in Covid-19 patients in variants so far encountered, the researchers said their results supported management measures to prevent thrombotic events, such as compression stockings or medical thromboprophylaxis drug treatments.
This was especially true for high-risk patients and strengthened the importance of vaccination against Covid-19, said the researchers from Umeå University.
Luckily, the peaks in the UK are starting to drop after the Winter and Spring peaks, but we may need to be aware that there may be an increase in DVT and related thrombotic events in the coming Winter.
They added, however, that more research was needed to establish whether Covid-19 increased the risk of PE or bleeding more than it does for other respiratory infections, such as flu.
In a related Editorial in the BMJ (4) Frederick Ho, PhD, and Jill Pell, MD, MBChB, both of the University of Glasgow in Scotland, said that the Swedish study findings are still clinically relevant, despite over 65% of the world's population having now received at least one COVID-19 vaccine dose at the time of writing the article. They say in their article:
"Current vaccines are highly effective against severe covid-19 but confer only moderate protection against infection with the omicron variant," they wrote. "Breakthrough infections are common, even after a third dose, and effectiveness against symptomatic disease appears to decrease to less than 50% 10 weeks after vaccination."
Ho and Pell said that while many Omicron infections are mild, the study shows that even un-hospitalized patients with mild cases are at increased risk for blood clots. "Mild disease accounts for a much larger proportion of infections (94.5% in this study)," they wrote. "This patient group may therefore contribute a substantial number of thromboembolic events."
References
Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study.
Lancet 2021;398:599-607. doi:10.1016/S0140-6736(21)00896-5 pmid:34332652
2. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study
BMJ 2022; 377 (Published 06 April 2022)Cite this as: BMJ 2022;377:e069590
3. Ioannis Katsoularis, Osvaldo Fonseca-Rodríguez, Paddy Farrington, Hanna Jerndal, Erling Häggström Lundevaller, Malin Sund, , Krister Lindmark, Anne-Marie Fors Connolly.
Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study
BMJ 2022; 377 Published 06 April 2022
4. Frederick Ho, PhD, and Jill Pell, MD, MBChB, both of the University of Glasgow in Scotland
Mayo Clin Proc 2021 Oct;96(10):2587-2597 pub 2021 Jul Thromboembolic Risk in Hospitalized and Nonhospitalized COVID-19 Patients: A Self-Controlled Case Series Analysis of a Nationwide Cohort
?Frederick K Ho 1, Kenneth K C Man 2, Mark Toshner 3, Colin Church 4, Carlos Celis-Morales 5, Ian C K Wong 2, Colin Berry 5, Naveed Sattar 5, Jill P Pell 6